Vitamin D Concentrations are Lower in Patients with Positive PCR for SARS-CoV-2
The world is currently gripped by the COVID-19 pandemic, which has been caused by the coronavirus strain SARS-CoV-2. Only a fraction of infected people show clinical symptoms, and an even lower percentage require medical attention. To date, it is not yet known why some patients develop more severe symptoms than others. A new study, published in Nutrients, and led by a team of scientists in Turin (Italy), investigated the potential relationship between vitamin D blood concentrations and SARS-CoV-2 infections.
D’Avolio et al. used the MassChrom® Vitamin D assay, automated on a MassSTAR automation system, to analyse 25-hydroxyvitamin D (25(OH)D) levels in the plasma of 107 patients who show symptoms of an acute respiratory disease, 27 of them infected with the virus. The authors demonstrate that SARS-positive tested patients had lower vitamin D levels than non-infected patients (Figure 1). The data did not show any statistically significant variations in the vitamin D levels between men and women.
However, when the groups of PCR negative and PCR positive patients were subdivided in to patients with an age below and above 70 years, 25(OH)D concentrations were only significantly lower in SARS-positive patients with an age greater than 70 years. This outcome might be important, given that age is a well-known predictor of disease severity.
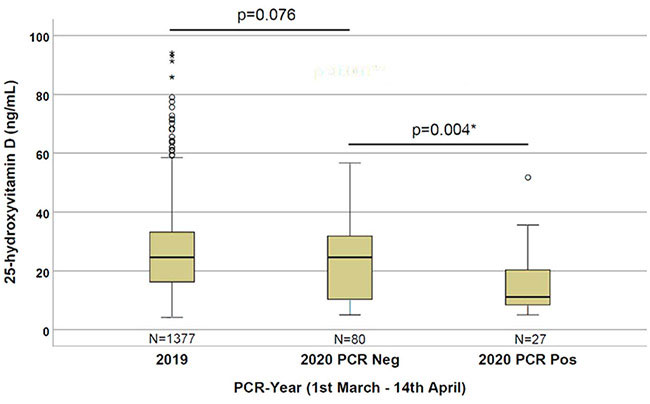
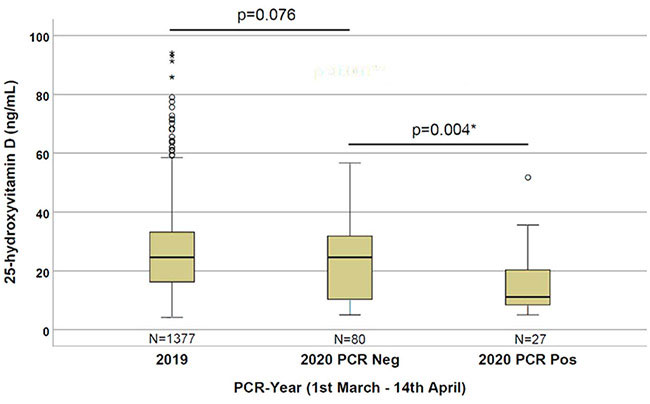
Figure 1: Patients that are PCR-positive for SARS-CoV-2 have a lower vitamin D level
One weakness of the study is the relatively low number of samples. However, the authors argue that their evidence is particularly strong because the group of non-infected patients was tested for the virus because there was a particular risk of infection, and they showed symptoms of a respiratory infection. The authors recognise the limitations of the study, in that patient samples are from a single hospital centre only and that they lack information about the severity of symptoms.
Why Vitamin D?
Vitamin D (1,25(OH)2D3) is known to play a key role in calcium metabolism and bone-formation, but it is also known to enhance the body’s immune response [1]. It possesses anti-inflammatory and immunoregulatory properties and is crucial for the activation of the immune system. Low levels of vitamin D have been shown to be associated with an increased susceptibility to infection and immune-related disorders [2]. For example, researchers found that low vitamin D levels increase the risk of respiratory diseases such as tuberculosis, asthma as well as viral and bacterial respiratory infections [3-6]. Vitamin D deficiency is also linked with decreased lung function, which may affect the body’s ability to fight respiratory infections [7]. Therefore, it would not be surprising if the risk of a SARS-CoV-2 infection is influenced by the vitamin D levels in a patient.
What could the study mean?
With the study of D’Avolio et al., it seems probable that vitamin D3 supplementation could be useful in the treatment of COVID-19 infections, for preventing a more severe symptomatology, and/or for reducing the presence of the virus in the upper respiratory tract — thus making patients less infectious. A paper by Grant et al. [9] suggests that people at risk of COVID-19 should consider taking 10,000 IU/day of vitamin D3 for a few weeks to rapidly increase their 25(OH)D concentrations, followed by 5000 IU/day to reduce the risk of infection. The goal should be to raise 25(OH)D concentrations above 40–60 ng/mL (100–150 nmol/L), or at least 30 ng/ml. However, D’Avolio et al. point out that randomised controlled trials and large population studies are now needed to confirm the preliminary observations presented in their study. As of July 2021, there are several trials ongoing. CORONAVIT in the UK is looking at whether correcting vitamin D deficiency during the winter will reduce the risk or severity of COVID-19 and other acute respiratory infections and includes 6,200 participants. In France, a smaller study, CoVitTrial, is trying to assess the impact of vitamin D on high-risk older adults. Results of both trials should be available later this year.
Last Update 14th December 2021
Original Study
References: